You've had four UTIs in the last six months.
Your doctor keeps prescribing antibiotics. You keep peeing after sex, chugging water, wearing cotton underwear. You're doing everything right.
And yet, two weeks after finishing your latest round of antibiotics, that familiar burning is back.
So what the hell is going on?
Here's what most doctors won't tell you: You might not be getting new UTIs. You might have one infection that never fully left.
There's a critical difference between recurrent UTIs and chronic UTIs—and understanding which one you have changes everything about how you should treat it.
Recurrent UTIs: The Revolving Door
Recurrent UTIs are what most women experience. These are distinct, separate infections caused by new bacterial invasions. You get infected, you treat it, it clears completely, and then—sometime later—you get infected again.
The technical definition: 3 or more UTIs in 12 months, or 2 or more in 6 months.
What's Happening:
Each infection is essentially starting from scratch. New bacteria (usually E. coli from your gut or introduced during sex) enter your urethra, travel up to your bladder, and set up shop.
Between infections, your urine cultures come back clean. You feel fine. Then something—sex, exercise, travel, stress—introduces new bacteria or disrupts your urogenital balance, and boom. Another UTI.
Why It Keeps Happening:
The problem with recurrent UTIs usually isn't that you're doing something wrong. It's that certain factors make you vulnerable to repeated infections:
1. Vaginal Microbiome Imbalance
Groundbreaking research from the University of Washington revealed that many women with recurrent UTIs have asymptomatic Bacterial Vaginosis (BV). Here's the mechanism:
- During sex, Gardnerella vaginalis (the bacteria responsible for BV) gets pushed into your urethra
- G. vaginalis damages and weakens your bladder wall cells
- This creates the perfect opportunity for E. coli to invade and multiply
Up to 84% of women with BV have no symptoms, which means you could have an imbalanced vaginal microbiome and not even know it.
2. The Antibiotic Trap
Every time you take antibiotics for a UTI, you're nuking your microbiome—both gut and vaginal. This:
- Reduces beneficial Lactobacillus populations in your vagina
- Raises vaginal pH (making it easier for bad bacteria to thrive)
- Increases your risk of BV
- Makes you more vulnerable to the next UTI
It's a vicious cycle: UTI → antibiotics → microbiome disruption → BV → another UTI.
3. Risk Factors You Can't Always Control
Some women are just more susceptible to recurrent UTIs due to:
- Anatomical differences (shorter urethra, proximity to anus)
- Hormonal changes (menopause, pregnancy)
- Sexual activity frequency
- Genetics
Chronic UTIs: The Infection That Won't Leave
Chronic UTIs are different. This isn't multiple infections—it's one persistent infection that never fully clears.
The bacteria aren't being completely eliminated by antibiotics. They're hiding. Waiting. And then resurfacing over and over again.
What's Happening:
The culprit is usually bacterial biofilm.
Biofilm is a protective shield that bacteria create to defend themselves from both your immune system and antibiotics. Think of it like bacteria building a fortress on your bladder wall.
Inside this biofilm:
- Bacteria can survive antibiotic treatment
- They remain dormant for weeks or months
- Standard urine cultures often miss them (because they're not free-floating in your urine)
- They can release from the biofilm, multiply, and cause "flare-ups" that feel like new infections
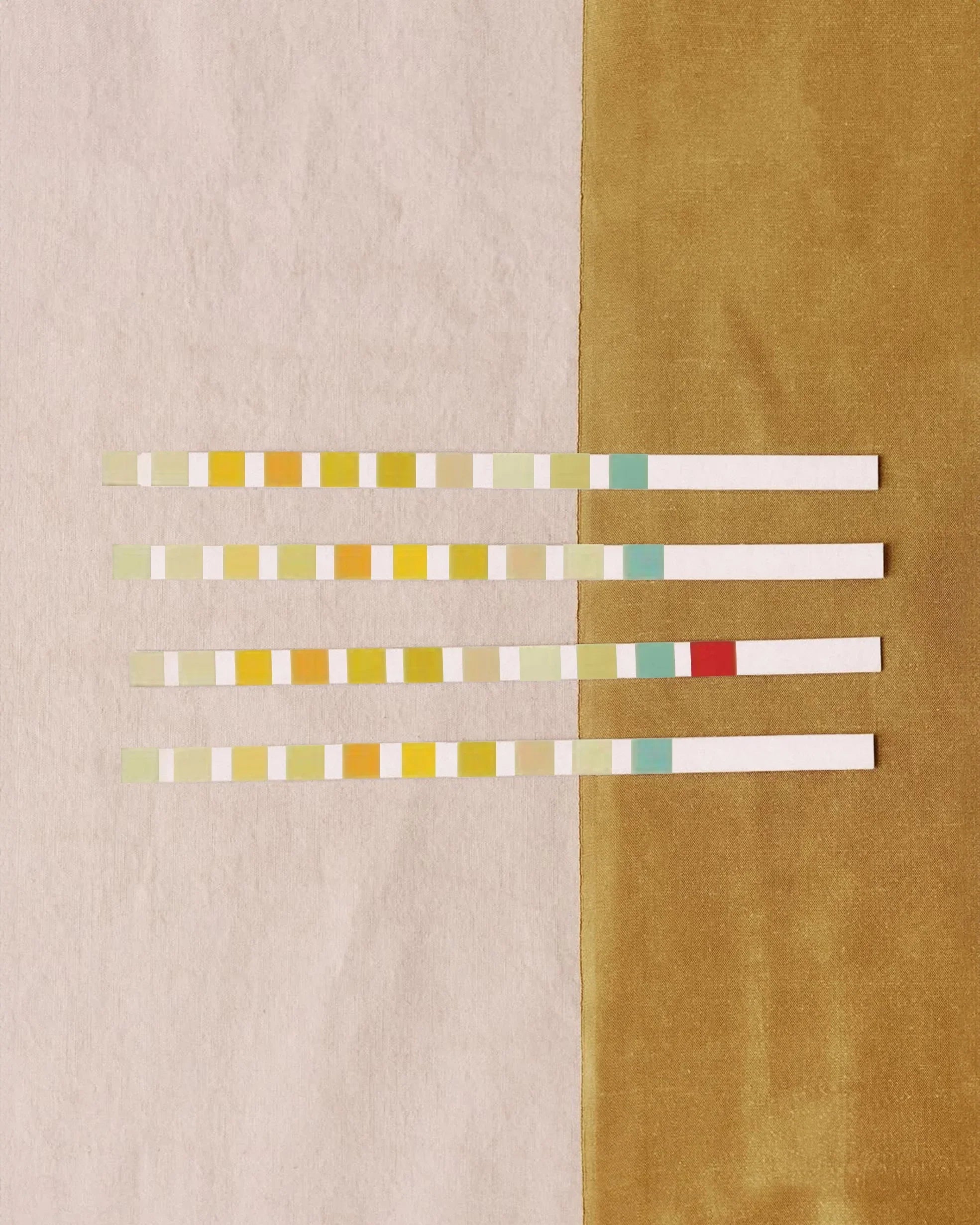
The Red Flags for Chronic UTI:
You might have a chronic UTI if:
✓ Your symptoms return within days or weeks of finishing antibiotics
✓ You have multiple negative urine cultures despite clear UTI symptoms
✓ Your UTIs always follow the same triggers (sex, exercise, stress)
✓ Antibiotics provide temporary relief but symptoms quickly return
✓ You have persistent bladder pain, urgency, or frequency even when cultures are "negative"
Research published in Microbiology Spectrum confirms that biofilms play a major role in chronic UTIs. This is why 30-44% of women who get one UTI will have another within six months—the first infection never fully left.
Why This Distinction Matters
Understanding whether you have recurrent or chronic UTIs completely changes your treatment approach.
For Recurrent UTIs:
Focus on prevention—stopping new bacteria from taking hold:
- Restore and maintain a healthy vaginal microbiome
- Use non-antibiotic preventives (like UTI Biome Shield with 100% bioavailable PACs)
- Address underlying risk factors (BV, hormonal imbalances)
- Support your immune system
For Chronic UTIs:
Focus on biofilm disruption—eliminating the bacteria that are already there:
- Longer courses of antibiotics (under medical supervision)
- Biofilm-disrupting agents
- Combination therapies that target both free-floating bacteria and biofilm colonies
- Bladder wall repair and immune support
Treating a chronic UTI like it's recurrent (short courses of antibiotics for each "flare") will never solve the problem. You're just temporarily suppressing symptoms without eliminating the source.
The Hidden Connection: Your Vaginal Microbiome
Here's what ties both types together: your vaginal health is directly connected to your urinary tract health.
Whether you're dealing with recurrent or chronic UTIs, an imbalanced vaginal microbiome makes everything worse.
The BV-UTI Cycle:
- You get a UTI and take antibiotics
- Antibiotics disrupt your vaginal microbiome
- Beneficial Lactobacillus populations decline
- G. vaginalis overgrows, causing BV (often with no symptoms)
- During sex, G. vaginalis damages your bladder wall
- This either introduces new E. coli (recurrent UTI) or reactivates dormant E. coli in biofilm (chronic UTI)
Breaking this cycle requires addressing both your urinary tract and your vaginal microbiome simultaneously.
Good Kitty's Dual-System Approach
After my 13th UTI in 2014, I wasn't just frustrated—I was desperate for answers. That's why we built UTI Biome Shield to address both recurrent and chronic UTIs through multiple mechanisms:
1. Prevent Bacterial Adhesion
- 100% bioavailable cranberry PACs (36mg per dose) block E. coli from sticking to your bladder wall
- Works whether bacteria are newly introduced or releasing from biofilm
2. Trap and Flush Bacteria
- D-mannose binds directly to E. coli fimbriae (the little hooks bacteria use to grab on)
- Acts like a decoy, trapping bacteria so they get flushed out when you pee
3. Disrupt Biofilm
- Specialized compounds target the protective shields bacteria hide behind
- Essential for chronic UTIs where biofilm is the primary issue
4. Support Microbiome Balance
- Prebiotics that feed beneficial bacteria
- Helps restore Lactobacillus populations in the vagina
- Reduces BV risk and breaks the UTI-antibiotic-BV cycle
5. Repair Bladder Tissue
- Vitamin D3 and zinc picolinate support tissue integrity and immune function
- Helps your bladder wall heal from repeated infections or G. vaginalis damage
What You Should Do Next
If You Have Recurrent UTIs:
1. Get tested for BV (even if you have no symptoms)
2. Focus on prevention with UTI Biome Shield or similar non-antibiotic options
3. Support your vaginal microbiome with targeted probiotics
4. Track your triggers (sex, exercise, diet) to identify patterns
If You Suspect Chronic UTI:
1. Talk to your doctor about the possibility of biofilm-related infection
2. Ask about longer antibiotic courses or combination therapies
3. Consider biofilm-disrupting supplements alongside medical treatment
4. Request a referral to a urologist or urogynecologist if standard treatment isn't working
The Bottom Line
You're not crazy. You're not dirty. You're not doing anything wrong.
UTIs—whether recurrent or chronic—are complex conditions that often require more than the standard "drink cranberry juice and pee after sex" advice.
Understanding the difference between getting new infections repeatedly and having one persistent infection that won't clear is the first step toward actually breaking the cycle.
Stop treating the symptoms. Start addressing the root cause.
— Meghan Carozza
Co-Founder & Chief Experience Officer, Good Kitty Co.
References:
- Kline, K.A., & Lewis, A.L. "Gram-Positive Uropathogens, Polymicrobial Urinary Tract Infection, and the Emerging Microbiota of the Urinary Tract." Microbiology Spectrum. 2016.
- Gilbert, N.M., et al. "Transient microbiota exposures activate dormant Escherichia coli infection in the bladder." PLOS Pathogens. 2017.
- CDC. "Bacterial Vaginosis Statistics." 2020.
- Brubaker, L., & Wolfe, A.J. "The female urinary microbiota, urinary health and common urinary disorders." Annals of Translational Medicine. 2021.
Read more
Advanced UTI Protection - While basic d-mannose supplements offer partial benefits, advanced formulations like Good Kitty's UTI Biome Shield with BioblocD3 technology represent the next generation ...

Learn to distinguish between UTI and overactive bladder symptoms, causes, and treatments. Stop misdiagnosis and find the right solution for your frequent urination.