Your vagina is an ecosystem. Here's how to be a good caretaker.
Let me introduce myself: I'm a vaginal ecologist.
No, seriously.
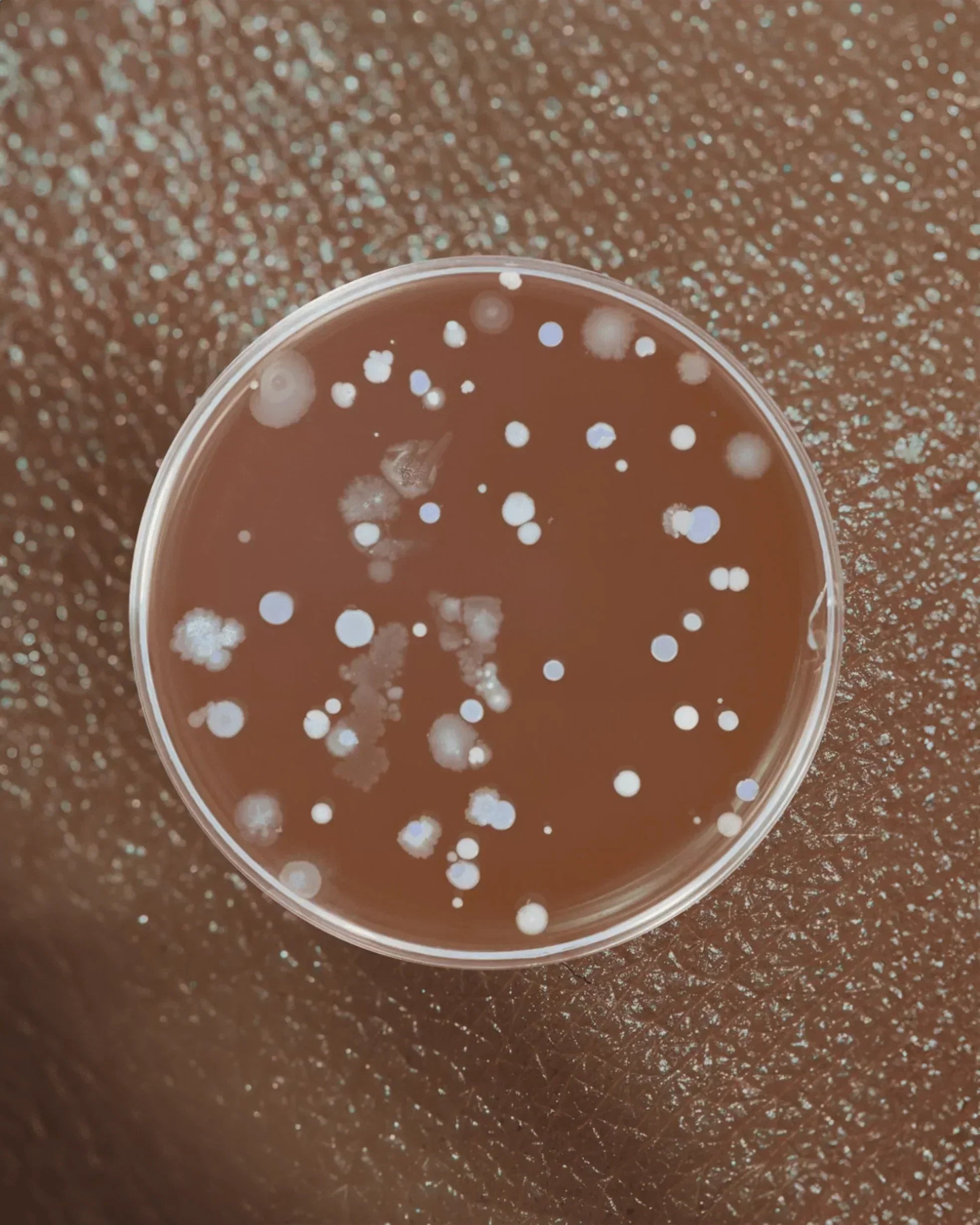
Just like your gut, your skin, and basically every other part of your body, your vagina has its own unique microbial environment—the vaginal microbiome.
And just like any ecosystem, when that delicate balance gets disrupted, shit goes sideways fast.
Here's what nobody tells you: Your vaginal health doesn't just affect your vagina. It affects:
🐱 Your risk of UTIs (spoiler: they're connected)
🐱 Your fertility
🐱 Your pregnancy outcomes
🐱 Your susceptibility to STIs (including HIV)
🐱 Your overall health
And yet, despite the fact that nearly one-third of women in the U.S. deal with bacterial vaginosis (BV) at some point, we're still expected to suffer in silence, cover up symptoms with scented products that make things worse, and accept whatever pharmaceutical band-aid gets thrown at us without asking questions.
Fuck that.
It's time to talk about what's actually going on down there, why it matters, and how to keep your vaginal ecosystem thriving—without relying on products that strip your health and make you dependent on more products.
Let's get into it.
Your Vagina Is an Ecosystem (And You Need to Treat It Like One)
Think of your vagina as a rainforest. A healthy rainforest has biodiversity—lots of different species living in balance, each playing a specific role in maintaining the health of the whole system.
Your vaginal microbiome works the same way.
When things are balanced, beneficial bacteria (primarily Lactobacillus species) dominate the landscape. They:
✔️ Keep vaginal pH low (acidic) by producing lactic acid
✔️ Prevent unfriendly yeasts, bacteria, and other organisms from taking over
✔️ Promote mucus production, creating a protective barrier against pathogens
✔️ Protect against infections—including UTIs, yeast infections, BV, and even HIV
When your vaginal flora is healthy, your vagina is actually cleaner than your mouth, according to Sharon Hillier, professor of obstetrics-gynecology at the University of Pittsburgh.
But when that ecosystem gets disrupted—through antibiotics, hormonal changes, diet, stress, sex, or any number of other factors—bad bacteria and yeasts can take over.
And that's when problems start.
The Lactobacillus Queens: Your Vagina's First Line of Defense
Lactobacillus bacteria are the queens of your vaginal microbiome.
These beneficial bacteria keep things running smoothly by:
🐱 Maintaining Acidic pH (3.8-4.5)
Lactobacillus produces lactic acid, which keeps your vaginal pH low and acidic.
Why this matters: E. coli (the bacteria responsible for 80-90% of UTIs) and other pathogens can't thrive in an acidic environment.
When your pH rises (becomes less acidic), it's like rolling out the red carpet for bad bacteria.
🐱 Creating a Protective Barrier
Lactobacillus promotes mucus production, which acts as a physical barrier against bacteria, yeasts, viruses (including HIV), and other pathogens trying to colonize your vaginal and urinary tissues.
🐱 Crowding Out the Competition
When Lactobacillus species dominate your vaginal microbiome, there's literally no room for harmful organisms to set up shop.
This is called competitive exclusion, and it's one of your body's most elegant defense mechanisms.
What Happens When Your Vaginal Ecosystem Gets Disrupted
When the balance of good bacteria gets thrown off—a condition called vaginal dysbiosis—you become vulnerable to a cascade of problems:
🚨 Bacterial Vaginosis (BV)
The most common vaginal infection, affecting nearly one-third of U.S. women.
Symptoms:
- Fishy odor (especially after sex)
- Thin, grayish-white discharge
- Irritation, itching, burning
The problem: BV isn't just annoying. It's linked to:
- Increased UTI risk
- Pelvic inflammatory disease
- Infertility
- Preterm labor
- Increased susceptibility to STIs (including HIV)
🚨 Recurrent Yeast Infections
When Lactobacillus populations drop, yeast (primarily Candida albicans) can overgrow.
Symptoms:
- Thick, white, cottage cheese-like discharge
- Intense itching
- Burning during urination or sex
- Redness and swelling
🚨 Chronic UTIs
Here's the connection nobody talks about: Vaginal dysbiosis is a major risk factor for recurrent UTIs.
When your vaginal pH rises and protective Lactobacillus populations decline:
- E. coli from your gut can colonize your vagina more easily
- During sex, these bacteria get pushed into your urethra
- Without an acidic vaginal environment to keep them in check, they travel to your bladder
Research shows that 84% of women with BV have no symptoms—meaning you could have vaginal dysbiosis increasing your UTI risk without even knowing it.
🚨 The BV-UTI Cycle
This is especially insidious:
- You get a UTI → treated with antibiotics
- Antibiotics kill good vaginal bacteria (Lactobacillus) along with bad
- Vaginal pH rises, bad bacteria overgrow (BV develops)
- During sex, Gardnerella vaginalis (the bacteria that causes BV) damages your bladder wall
- This reactivates dormant E. coli hiding in biofilms OR introduces new bacteria
- You get another UTI → more antibiotics → worse dysbiosis
And the cycle continues.
🚨 Other Consequences of Vaginal Dysbiosis
- Chronic pelvic pain
- Painful sex
- Vaginal dryness
- Group B Strep infections
- Infertility and IVF failure
- Recurrent miscarriage
- Preterm birth
- Increased risk of PCOS, endometriosis
- Higher susceptibility to environmental toxins
Your vaginal microbiome isn't just about vaginal health. It's a barometer for your overall health.
When your vaginal ecology is regularly imbalanced, it's likely your gut microbiome is too.
What Disrupts Your Vaginal Ecosystem
Let's talk about the culprits that throw your vaginal microbiome out of balance:
🚫 1. Antibiotics
Antibiotics are lifesaving when you need them. But they're also indiscriminate killers—they wipe out good bacteria along with bad.
Even one round of antibiotics for a UTI can trigger recurrent vaginal yeast infections that last for months.
What to do:
- Avoid unnecessary antibiotic use whenever possible
- If you must take antibiotics, take a probiotic alongside them (containing Lactobacillus, Bifidobacterium, and Saccharomyces species)
- Continue the probiotic daily for up to 3 months after finishing antibiotics
🚫 2. Hormonal Birth Control
Oral contraceptives can disrupt vaginal pH and flora balance.
For some women, this isn't a problem. For others, it triggers chronic yeast infections or BV.
🚫 3. Spermicides and Chemical Lubricants
Products containing nonoxynol-9 (found in spermicides and spermicidal condoms) dramatically alter vaginal pH and kill beneficial Lactobacillus.
Most commercial lubricants contain:
- Glycerin (a sugar that feeds yeast)
- Parabens
- Fragrances
- Other chemicals that disrupt pH
What to use instead:
- Non-spermicidal condoms (like Sustain brand)
- pH-balanced, water-based or aloe-based lubricants without glycerin, parabens, or fragrances
🚫 4. Douches, Scented Products, and "Feminine Hygiene" Products
Your vagina is self-cleaning. It does not need "freshening."
Douches, scented sprays, perfumed pads/tampons, and "feminine wipes" all:
- Disrupt vaginal pH
- Kill beneficial bacteria
- Introduce irritants and chemicals
- Make infections MORE likely, not less
Never douche. Ever.
🚫 5. Non-Organic Menstrual Products
Most conventional pads and tampons contain:
- Bleach residues
- Pesticide residues
- Synthetic fibers
- Fragrances
All of these can irritate delicate tissue and disrupt your microbiome.
What to use:
- Organic cotton pads and tampons
- Menstrual cups (medical-grade silicone)
- Period underwear (PFAS-free brands only—see our article on PFAS)
🚫 6. Sugar and Refined Carbohydrates
High sugar intake and refined carbs feed yeast and disrupt gut flora, which in turn affects vaginal flora.
Pre-diabetes and diabetes are major risk factors for recurrent yeast infections.
But even if you're not diabetic, eating too much sugar—including alcohol, which acts as sugar in your body—can trigger infections.
For some women with recurrent yeast infections, even excessive fruit, honey, and dates can be problematic.
What to do:
- Eliminate added sugars and refined carbs until you've been infection-free for 6+ months
- Emphasize protein, healthy fats, and fiber-rich vegetables
- Keep blood sugar stable
🚫 7. Gut Dysbiosis
Your gut health directly affects your vaginal health.
Imbalances in gut flora (intestinal dysbiosis) are a root cause of chronic or recurrent vaginal infections.
What to do:
- Eat 6-8 servings of vegetables daily (especially leafy greens)
- Include resistant starches (sweet potatoes, legumes)
- Eat lactofermented foods daily (sauerkraut, kimchi, yogurt, kefir)
- Take a probiotic containing Lactobacillus reuteri, L. rhamnosus, and L. crispatus (all vagina-friendly strains)
🚫 8. Sex (Depending on the Circumstances)
Sex itself isn't the problem. But certain aspects of sexual activity can disrupt vaginal ecology:
Risk factors:
- Multiple or new sexual partners
- Frequent sex without adequate lubrication
- Oral sex (can dramatically change vaginal pH)
- Semen (alkaline pH can temporarily raise vaginal pH)
- Partners harboring bacteria (men can carry bacteria asymptomatically)
What to do:
- Use condoms (non-spermicidal)
- Use vagina-friendly lube
- Pee after sex
- Consider taking a probiotic orally or inserting vaginally around times of high sexual activity
🚫 9. Hormonal Changes
Menstruation, pregnancy, and menopause all cause pH changes that can reduce Lactobacillus and allow overgrowth of yeast or BV.
Yeast infections are especially common:
- Around your period
- During pregnancy (higher blood sugar + hormonal changes)
BV is especially common:
- During menopause (dropping estrogen changes vaginal pH and tissue health)
What to do:
- Take a probiotic during high-risk times (menstruation, pregnancy, perimenopause)
- Avoid blood sugar spikes
- Use condoms during menopause (semen's alkaline pH + reduced estrogen = perfect BV recipe)
🚫 10. Poor Hygiene Habits
Wiping back to front after a bowel movement transfers bacteria from your rectum to your vagina.
Same with vaginal contact after anal sex (fingers, penis, toys—anything).
What to do:
- Always wipe front to back
- No vaginal contact after anal contact without thorough washing or barrier change
How to Keep Your Vaginal Ecosystem Thriving
Okay, so now you know what NOT to do. Here's what you SHOULD do to maintain a healthy vaginal microbiome:
✔️ 1. Feed Your Good Bacteria
Your microbiome thrives on:
- Fiber (6-8 servings of vegetables daily)
- Resistant starches (sweet potatoes, legumes, lentils)
- Fermented foods (yogurt, kefir, sauerkraut, kimchi)
✔️ 2. Take a Quality Probiotic
Look for one containing:
- Lactobacillus reuteri
- Lactobacillus rhamnosus
- Lactobacillus crispatus
- Bifidobacterium species
- At least 10 billion CFUs
✔️ 3. Get Your Vitamins
Healthy vaginal tissue requires:
- Zinc
- Vitamin A
- Vitamin E
- Vitamin C
Get these through diet (protein, nuts, seeds, colorful vegetables) or a high-quality multivitamin.
✔️ 4. Choose Products Carefully
Condoms: Non-spermicidal (Sustain brand is excellent)
Lube: pH-balanced, water- or aloe-based, no glycerin/parabens
Menstrual products: Organic cotton only
Sex toys: Medical-grade silicone, glass, or stainless steel; wash thoroughly before and after use
✔️ 5. Support Your Gut Health
Remember: gut health = vaginal health.
If you struggle with digestive issues, chronic infections, or other signs of gut dysbiosis, addressing your gut microbiome is essential.
✔️ 6. Manage Blood Sugar
Keep blood sugar stable by:
- Eating protein with every meal
- Avoiding refined carbs and added sugars
- Not skipping meals
- Managing stress
✔️ 7. Avoid Unnecessary Antibiotics
Use natural remedies when possible. When antibiotics are necessary, protect and restore your microbiome with probiotics for 3 months afterward.
The UTI-Vaginal Health Connection
Here's why this all matters for UTI prevention:
A healthy vaginal microbiome is your first line of defense against UTIs.
When Lactobacillus populations are strong:
- Vaginal pH stays low (acidic)
- E. coli can't colonize your vaginal or urethral tissue
- Protective mucus barriers prevent bacterial adhesion
- Your immune system functions optimally
When vaginal dysbiosis occurs:
- pH rises (becomes less acidic)
- E. coli and other pathogens can thrive
- During sex, these bacteria get pushed into your urethra
- You get a UTI
This is why Good Kitty's UTI Biome Shield includes ingredients that support both urinary AND vaginal microbiome health:
🐱 100% bioavailable cranberry PACs – Prevent bacterial adhesion
🐱 D-mannose – Traps E. coli for elimination
🐱 Vitamin D3 and zinc – Support immune function and tissue health
Combined with a healthy vaginal microbiome, this multi-mechanism approach gives you comprehensive protection against UTIs.
The Pharmaceutical Problem
Before we wrap up, let's talk about why I'm not recommending the latest FDA-approved pharmaceutical for BV.
This week, the FDA approved Secnidazole (Solosec)—a one-dose treatment for bacterial vaginosis.
Sounds convenient, right?
Here's the problem:
❌ Approved based on only 333 women studied
❌ Can cause vaginal yeast infections that require additional treatment
❌ The FDA admits it's a carcinogen that caused tumors in mice—and they don't know if a single dose causes cancer in humans
Let me say that again: The FDA approved a known carcinogen for use in women, based on a study of just 333 people, with no long-term safety data.
We're not that far from the DES nightmare (a drug given to pregnant women that caused cervical cancer in their daughters and cancer in their sons).
You are not a guinea pig for Big Pharma.
The "Chase Rule of 3" from Yale School of Medicine states: Never use a medication until it's been on the market for at least 3 years because post-market surveillance is where we often discover the ugly truths about safety.
Pharmaceuticals don't restore vaginal ecology. They're temporary band-aids that don't address root causes.
You deserve better.
The Bottom Line
Your vagina is an ecosystem that requires care, respect, and balance.
When that ecosystem is healthy: ✔️ You're protected against UTIs, yeast infections, and BV
✔️ Your fertility is supported
✔️ Your pregnancy outcomes are better
✔️ Your overall health improves
When it's disrupted: ❌ You're vulnerable to infections
❌ You end up in cycles of antibiotics and repeat infections
❌ Your health—reproductive, urinary, and overall—suffers
The good news? You have more control than you think.
By:
- Feeding your good bacteria
- Avoiding products and habits that disrupt your microbiome
- Supporting gut health
- Taking targeted probiotics
- Making informed choices about sex, birth control, and menstrual products
You can maintain a thriving vaginal ecosystem—and break free from the infection-antibiotic-repeat cycle.
There's no advocacy group for keeping our vaginas healthy.
So we have to be our own advocates.
And it starts with understanding that your vagina isn't just a body part—it's an ecosystem that deserves your attention, respect, and care.
— Meghan Carozza
Co-Founder & Chief Experience Officer, Good Kitty Co.
References:
- Hillier S. "The vaginal microbiota and urinary tract infection." University of Pittsburgh Department of Obstetrics-Gynecology.
- Reno H. "The Superhero in Your Vagina." The Atlantic.
- Stapleton AE. "The vaginal microbiota and urinary tract infection." Microbiology Spectrum. 2016.
Note: For comprehensive information on treating BV and yeast infections naturally, check out Botanical Medicine for Women's Health by Dr. Aviva Romm. Good Kitty focuses on UTI prevention, but we believe all women deserve complete information about their vaginal and urinary health.
Read more

Your period is more than a monthly inconvenience—it’s a vital sign. Learn what your cycle reveals about hormones, thyroid health, stress, and overall wellbeing.

BV and yeast infections can flare after antibiotics, sex, or even the wrong lubricant. Here’s what actually causes imbalance—and how gentle, science-backed support like UTI Biome Shield can help ke...







Leave a comment
All comments are moderated before being published.
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.